
Free Organisational Tools for New Doctors
Being organised is key to being efficient, particularly when dealing with a high workload.
I’ve created some FREE organisational tools for new doctors which you can download below.
On-Call Referrals Pro forma
This form is designed for use during on-call shifts to document referrals you receive.

How to use the On-Call Referrals Proforma
At the top of each box there is space to take down patient details. You’d be amazed how often people forget to volunteer information like the patient’s name or the ward they are on, especially when they are stressed.
Once you’ve filled in the patient identifiers you should take down the details of the referral using the SBAR communication tool.
SBAR stands for:
- Situation
- Background
- Assessment
- Recommendation
According to NHS England and NHS Improvement:
“SBAR helps to provide a structure for an interaction that helps both the giver of the information and the receiver of it. It helps the giver by ensuring they have formulated their thinking before trying to communicate it to someone else. The receiver knows what to expect and it helps to ensure the giver of information is not interrupted by the receiver with questions that will be answered later on in the conversation.”
Using an SBAR communication tool looks something like this:
Situation:
I am (name), (X) nurse on ward (X)
I am calling about (patient X)
I am calling because I am concerned that… (e.g. BP is low/high, pulse is XX, temperature is XX, Early Warning Score is XX)
Background:
Patient (X) was admitted on (XX date) with… (e.g. MI/chest infection)
They have had (X operation/procedure/investigation)
Patient (X)’s condition has changed in the last (XX mins)
Their last set of obs were (XX)
Patient (X)’s normal condition is… (e.g. alert/drowsy/confused, pain free)
Assessment:
I think the problem is (XXX)
And I have… (e.g. given O2/analgesia, stopped the infusion)
OR I am not sure what the problem is but patient (X) is deteriorating
OR
I don’t know what’s wrong but I am really worried
Recommendation:
I need you to…
Come to see the patient in the next (XX mins)
AND
Is there anything I need to do in the mean time? (e.g. stop the fluid/repeat the obs)
Taken from: Quality, Service Improvement and Redesign Tools: SBAR communication tool – situation, background, assessment, recommendation
Try to use this format when communicating clinical information and encourage others to do the same. The pro forma should help to keep information you receive about patient referrals organised.
Task Prioritisation Tool
This is a task prioritisation tool I myself use when receiving handover for ward patients. The theory behind this tool is the prioritisation of tasks by clinical urgency which is a core skill all doctors need to develop. At the beginning of your medical career, it can be hard to know which task is more clinically urgent. What I’ve tried to do here is give you a list of clinical tasks moving from most urgent (Category 1) to least urgent (Category 8). This is especially useful at weekends when the clinical team is smaller and therefore the workload per doctor is higher and you may be delegated multiple types of tasks.
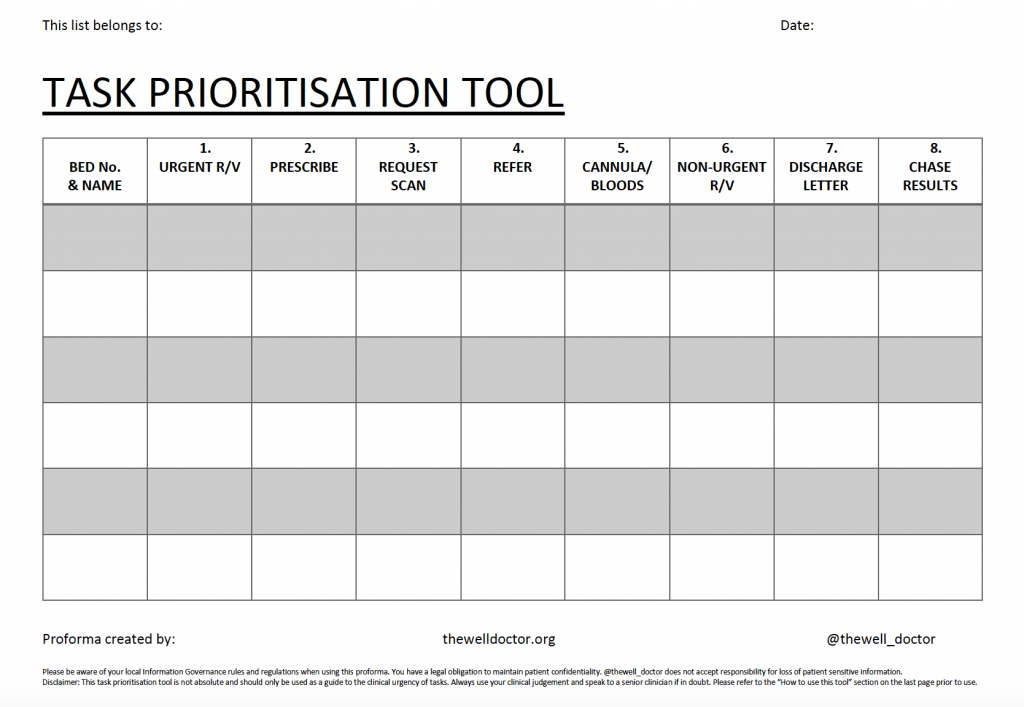
How to use the tool
Use the first column to document names and bed spaces for the patients on the ward. During the handover tick which tasks are required for the patient in the relevant columns.
The Categories are:
- Urgent Review: Assess any patients who are unwell/ urgently need review
- Prescribe: Prescribe any medications that need to be prescribed
- Request scan: Request urgent scans
- Refer: Call other specialists for referrals that need to be made or to ask for advice
- Cannula/ Bloods: Do any urgent blood tests/ insert cannulas for those who need them (especially when the next dose of IV medication is looming – consider noting a time when the next dose of IV medication is due)
- Non-Urgent Review: Review other patients who need less urgent reviews throughout the day – remember to note a time so you know who to see first!
- Discharge letters: Write discharge letters / do paperwork
- Chase results: Chase any outstanding results for patients
You can use the space in each box to add details about the task e.g. type of scan, specialist to refer to, list of blood tests requested. Focus in the tasks in column one, before moving to column 2 etc to prioritise your day. You should aim to complete tasks in Category 1 before moving across from left to right. During the day you can add to the tasks for each patient, which should prompt you to go back to Category 1 and work your way back across.
Examples:
- An unwell patient who needs urgent review will clearly be a greater priority than doing discharge letter paperwork.
- Prescription of new medications is important so the nurses can administer these as soon as possible.
- Requesting scans and speaking to other specialties should be done as early as possible to increase the likelihood of getting scans done on the day of the request and to allow other specialties enough time to review your patient.
Disclaimer: This list is not absolute
Example 1:
Phlebotomy including venepuncture and cannulation should be done early so you can get test results back quickly and administer medications as soon as possible. However, the exact urgency will depend on the clinical state of the patient. If the patient is clinically stable and/or IV medication is not due for a while, these procedures can be done in Category 5. If, on the other hand, the patient is clinically unstable then these procedures should form part of the initial management plan when you do your urgent review for an unwell patient – and so move to Category 1.
Example 2:
Chasing non-urgent results can often wait until later in the day and discharge paperwork may take precedence so that bed spaces can be created. However, if you suspect someone may have had a myocardial infarction for example, you would want to chase the result (usually Category 8) for troponin much sooner as it will inform the management of an unwell patient (Category 1).
Always use your own clinical judgement to prioritise the urgency of clinical tasks and ask seniors when in doubt. If a senior clinician delegates a specific task to you and/or deviates from the order above, defer to their expertise.
A Note on Confidentiality:
Please take care of any documents which contain patient sensitive information. You have a legal duty as a clinician to protect patient confidentiality. You must make sure any personal information about patients that you hold or control is effectively protected at all times against improper access, disclosure or loss. You should not leave patients’ records, including the information in these forms, unattended. Notes and records may be seen by other patients, unauthorised staff, or the public if they are not managed securely.
I hope you enjoy using these tools! Staying organised by keeping an accurate record of referrals and prioritising your clinical tasks by type/ urgency instead of by patient/ bed-space should help make working days easier and allow you to re-prioritise as necessary.
Have you tried these tools? What did you like about them? What do you think could be improved?
Let me know in the comments, I would love to hear from you.
Sign up for our newsletter





